To see the full paper click here:
To see the commentary click here:
Bluesky thread:
Let me tell you about the #BowdishLab & friend’s most recent paper “Neutrophil-mediated innate immune resistance to bacterial pneumonia is dependent on Tet2 function”, led by Dr. C. Quin (now at @uniofaberdeen.bsky.social) @jclinical-invest.bsky.social https://www.jci.org/articles/view/171002
Tet2 is gene that is involved with methylating genes and therefore changing gene expression. Sometimes spontaneous mutations of Tet2 in hematopoetic stem cells (HSC) occur. These mutants tend to produce more myeloid cells (monocytes/neutrophils).
These myeloid producing HSCs tend to be more fit in the aging bone marrow (Darwinian survival of the fittest) and overtime, more and more of your myeloid cells are made from these Tet2 mutant clones.
In extreme cases this can lead to myelodysplastic disorders or cancer, but sub-clinical CHIP or clonal hematopoeisis of indeterminant potential occurs in many older adults.
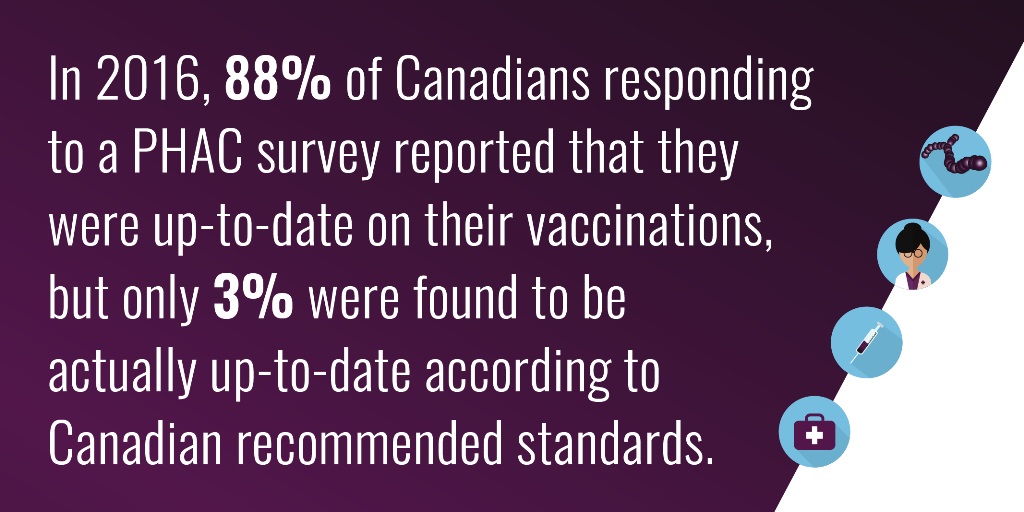
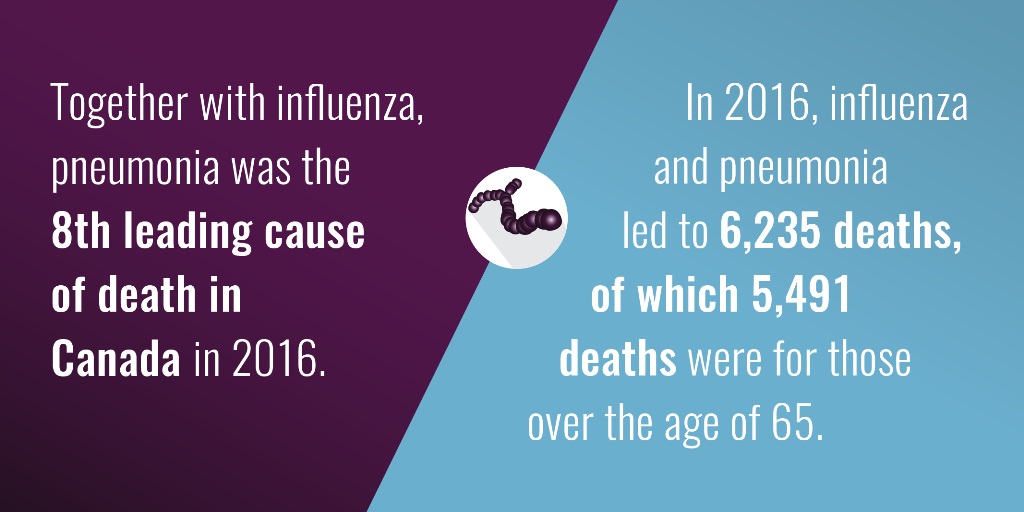
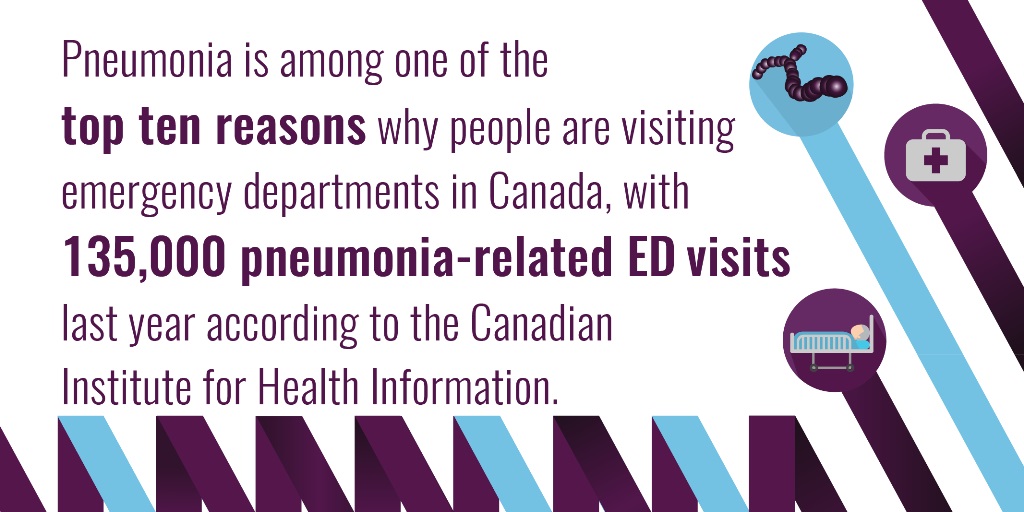
People with CHIP (i.e., too many of their myeloid cells are made from Tet2 mutant progenitors) are prone to all sorts of conditions (e.g., heart disease) and pneumonia. We hypothesized that pneumonia risk might be due to changes in innate immune/myeloid cell function.
Mice defective in Tet2 did very poorly during Streptococcus pneumoniae infection (the most common cause of community acquired pneumonia in older adults), because their neutrophils were less able to kill bacteria.
We are excited about this @jclinical-invest.bsky.social publication because it is the first mechanistic explanation for the increased risk of pneumonia in CHIP. Generally CHIP is thought to affect macrophage function, but it clearly affects neutrophil gene expression & function as well.
Many thanks to Dr. Elsa Bou Ghahem for her most excellent Commentary https://www.jci.org/articles/view/181064 and for the great editorial & reviewer experience @jclinical-invest.bsky.social
Research Team:Candice Quin, Erica N. DeJong, Elina K. Cook, Yi Zhen Luo, Caitlyn Vlasschaert, Sanathan Sadh, Amy J.M. McNaughton, Marco M. Buttigieg, Jessica A. Breznik, Allison E. Kennedy, Kevin Zhao, Jeffrey Mewburn, Kimberly J. Dunham-Snary, Charles C.T. Hindmarch, Alexander G. Bick, Stephen L. Archer, Michael J. Rauh, Dawn M.E. Bowdish